Let’s be honest. For a long time, the conversation around plastic surgery was… superficial. It was about vanity, celebrity culture, and erasing wrinkles. But the real story, the one happening in surgeons’ offices and patients’ lives every single day, is far more complex. It’s a story deeply intertwined with mental health.
This isn’t about good or bad. It’s about nuance. It’s about understanding that a scalpel can be a tool for profound psychological transformation—or a dangerous trigger for deeper issues. So, let’s dive in and unpack this complicated, fascinating relationship.
The Psychological Boost: When Surgery Heals the Inside, Too
For many, the decision to go under the knife isn’t a whim. It’s a calculated step toward feeling more like themselves. The psychological benefits of plastic surgery, when done for the right reasons, can be incredible.
Reconstructing Confidence
Think about someone who has survived breast cancer. A mastectomy is life-saving, but it can also be a brutal assault on a person’s identity and femininity. Breast reconstruction isn’t just about restoring a physical form; it’s about restoring a sense of wholeness. The relief, the regained confidence—that’s a mental health outcome as much as a physical one.
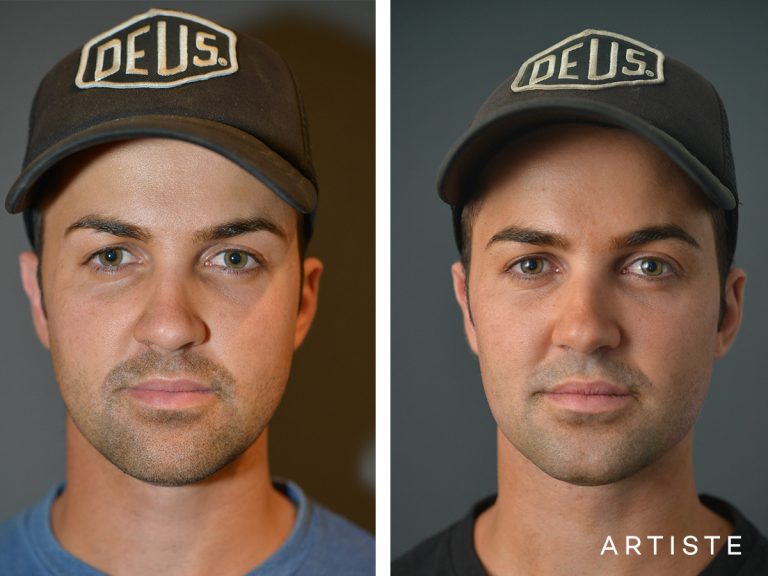
Correcting a Lifelong Insecurity
Now, consider someone who has been teased their entire life about a prominent nasal hump or ears that stick out. That constant, low-grade humiliation can chip away at self-esteem. For these individuals, a rhinoplasty or otoplasty isn’t about becoming someone else. It’s about aligning their outer appearance with how they feel on the inside. The result? Often, a dramatic drop in social anxiety and a newfound willingness to engage with the world.
In these cases, the surgery acts as a key that unlocks a door to better mental well-being. It removes a constant source of stress, allowing a person to focus their energy on living instead of hiding.
The Other Side of the Coin: The Mental Health Risks
And yet, here’s the deal. Plastic surgery is not a magic wand for happiness. If the source of a person’s unhappiness is internal, no external change will fix it. This is where things can get dangerously murky.
Body Dysmorphic Disorder (BDD): The Red Flag
The biggest red flag for any ethical plastic surgeon is Body Dysmorphic Disorder. BDD is a mental health condition where a person becomes obsessively preoccupied with a perceived flaw in their appearance—a flaw that is often minor or not observable to others.
A patient with BDD might seek surgery to “fix” their imagined defect. But the surgery never helps. In fact, it almost always makes things worse. The obsession simply shifts to another body part, leading to a heartbreaking and dangerous cycle of repeated procedures, financial ruin, and psychological devastation. Ethical surgeons are trained to screen for BDD and will often refuse surgery, instead recommending psychological support.
Unrealistic Expectations and “Post-Surgery Depression”
Even for patients without BDD, unrealistic expectations are a major pitfall. If someone believes a new nose will land them their dream job and a perfect relationship, they are setting themselves up for a crash. Surgery comes with swelling, bruising, and a lengthy recovery period. This can trigger a temporary state often called “post-surgery blues,” where patients question their decision amidst the discomfort.
Without proper mental preparation, this can deepen into a more significant depression. The “new you” arrives, but the old problems are still there, waiting.
The Ideal Pathway: Where Mental and Physical Health Collaborate
So, what does a healthy approach to plastic surgery and mental wellness look like? It looks like collaboration. It looks like integration.
The Critical Role of the Surgeon-Patient Consultation
The first line of defense is a thorough, compassionate consultation. A good surgeon won’t just measure your features; they’ll try to measure your motivations. They’ll ask:
- “Why are you considering this procedure now?”
- “What are your specific hopes for the outcome?”
- “How do you think your life will change afterwards?”
Their job is to separate healthy desires from unhealthy fixations. They are gatekeepers, in a sense, for the patient’s own well-being.
The Growing Trend of Psychological Screening
More and more, the field is recognizing the need for formal psychological evaluation before major elective procedures. This isn’t about judging a patient “crazy.” It’s about ensuring they are emotionally prepared for the journey and that their goals are realistic. It’s a sign of a responsible, modern practice.
Aftercare: The Often-Forgotten Component
Mental health support shouldn’t end when the bandages come off. The best outcomes involve ongoing check-ins, not just on the physical healing but on the emotional adjustment to a changed appearance. Some forward-thinking clinics even have therapists on staff or have partnerships with them.
A Final Thought: The Mirror and the Mind
Plastic surgery, at its best, is a powerful tool. It can correct, restore, and empower. But it is not a substitute for therapy, self-love, or inner work. The goal should never be perfection—that’s a phantom that can never be caught.
The real transformation happens when the change on the outside finally lets the person on the inside breathe a sigh of relief and step forward into the world. It’s about congruence. It’s about peace. And achieving that, well, that requires looking as honestly at the reflection in your mind as the one in the mirror.