You’ve probably heard of the low-FODMAP diet as a lifeline for IBS sufferers—but what if its benefits stretch further? Turns out, this eating plan might be a secret weapon for general digestive wellness, even if you don’t have a formal diagnosis. Let’s unpack why.
What Exactly Are FODMAPs?
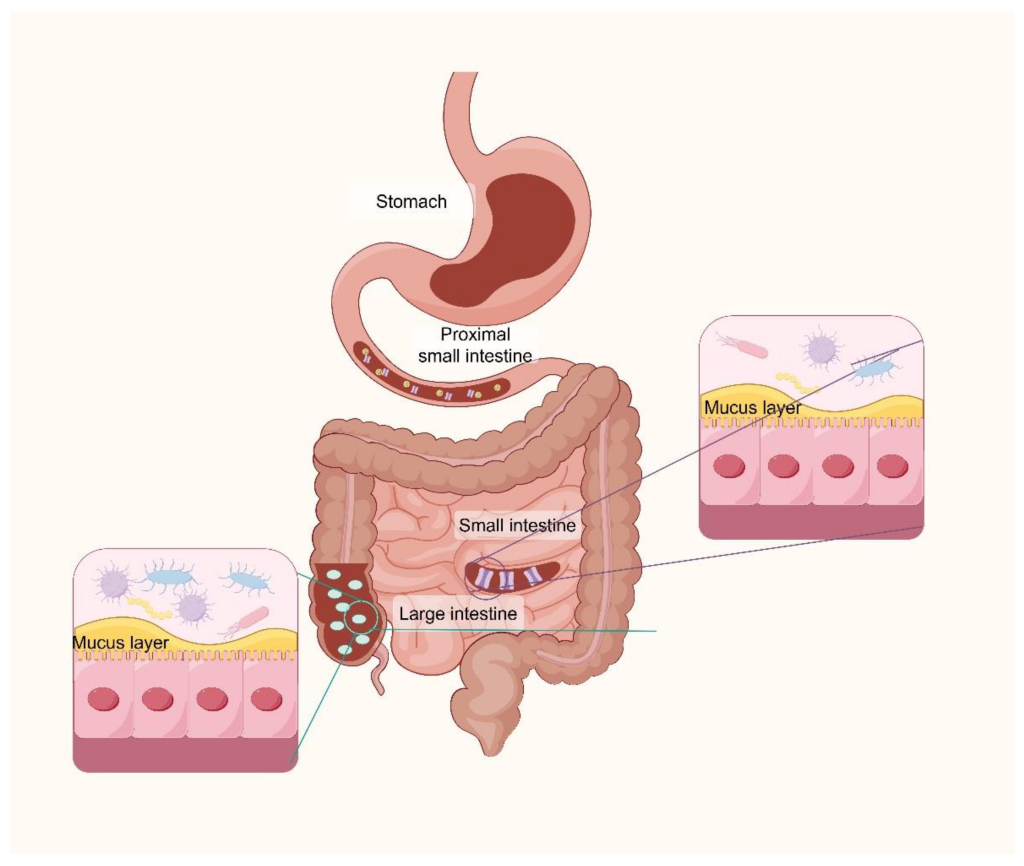
FODMAPs—Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols—are short-chain carbs that some guts struggle to absorb. Think of them like uninvited party guests: they ferment in your colon, causing bloating, gas, and discomfort for sensitive folks.
Common High-FODMAP Offenders
- Oligosaccharides: Wheat, onions, garlic, legumes
- Disaccharides: Lactose (dairy like milk, soft cheeses)
- Monosaccharides: Excess fructose (apples, honey, mangoes)
- Polyols: Sugar alcohols (sorbitol in stone fruits, artificial sweeteners)
Why Low-FODMAP Works for More Than Just IBS
Sure, it’s gold-standard for IBS management—but here’s the twist: digestive distress doesn’t always fit neat diagnostic boxes. Many people experience “functional” bloating, irregularity, or discomfort without a clear cause. A low-FODMAP approach can act like a reset button.
The Gut Microbiome Connection
Emerging research suggests FODMAPs influence gut bacteria balance. For some, reducing them temporarily may ease dysbiosis (microbial imbalance)—a hot topic in gut health circles. It’s not about banning these foods forever, but giving your system breathing room.
Inflammation and Sensitivity
Chronic low-grade inflammation can make guts hypersensitive. By dialing down FODMAPs—which can irritate an already angry gut—you might reduce overall digestive inflammation. Think of it like turning down the volume on a staticky radio.
Who Else Might Benefit?
Beyond IBS, these scenarios could signal FODMAP sensitivity:
- Unexplained bloating after meals (even “healthy” ones)
- Cycling through “trigger foods” without clear patterns
- Histamine intolerance or mast cell activation overlaps
- Post-infectious gut issues (like after food poisoning)
How to Try Low-FODMAP Without the Overwhelm
Here’s the deal: this isn’t a forever diet. It’s a detective tool. Follow these steps to avoid common pitfalls:
- Elimination Phase: 2-6 weeks of strict low-FODMAP foods (use Monash University’s app for accuracy)
- Reintroduction: Test one FODMAP group at a time (e.g., fructose first, lactose next)
- Personalization: Keep only the problem triggers, liberalize the rest
Pro Tips for Success
- Don’t skip reintroduction—permanent restriction risks nutrient gaps
- Work with a dietitian if you have a history of disordered eating
- Watch for “FODMAP stacking” (multiple low-FODMAP foods adding up)
The Surprising Side Benefits
Beyond belly comfort, many report unexpected wins:
- Fewer energy crashes (less post-meal fermentation = steadier energy)
- Clearer skin (gut-inflammation-skin axis at play)
- Improved sleep (discomfort → restlessness connection)
When Low-FODMAP Isn’t the Answer
It’s not a cure-all. Red flags that something else is going on:
- Weight loss without trying
- Blood in stool
- Severe pain waking you at night
Final Thoughts: A Tool, Not a Religion
The goal isn’t perfection—it’s digestive peace. For some, that means identifying two trigger foods; for others, a seasonal reset. Listen to your gut (literally). Because sometimes, the best diet is the one you barely notice… except by its absence.